Remote patient monitoring (RPM) is a telehealth service that allows qualified healthcare professionals and patients to manage acute and chronic conditions. RPM helps prevent health complications and improve patient outcomes. But who qualifies for remote patient monitoring, and how can healthcare providers implement RPM?
Who Qualifies for Remote Patient Monitoring?
The Centers for Medicare and Medicaid Services (CMS) defines remote patient monitoring as “the use of digital technologies to collect health data from patients in one location and electronically transmit that information securely to providers in a different location (data can include vital signs, weight, blood pressure, blood sugar, pacemaker information, etc.).” Who qualifies for remote patient monitoring is noted by CMS as the following.
- Individuals with chronic conditions like diabetes, hypertension, heart disease, asthma, or COPD.
- Post-surgical patients who need to monitor their recovery and wound healing.
- Geriatric patients, particularly those with multiple chronic conditions or limited mobility.
- Patients in rural or remote areas have difficulty accessing in-person care.
- Patients with acute conditions that require close monitoring, such as COVID-19.
Who Performs Remote Patient Monitoring Services?
There are many remote patient monitoring use cases, from prevention to surgical recovery. Remote patient monitoring services must be ordered and billed only by physicians or non-physician practitioners. That includes qualified physicians and healthcare professionals such as nurse practitioners, certified nurse specialists, or physician assistants. The practitioners must be eligible to bill Medicare for evaluation and management services.
A qualified healthcare professional must have a relationship with the patient to order remote patient monitoring services. In the case of a new patient, an in-person examination is required before enrolling in an RPM program. Patients who qualify for RPM use medical devices that measure and transmit their physiologic data to their providers. The following section explains which devices allow for remote patient monitoring services.
Which RPM Devices Qualify for Remote Patient Monitoring?
Remote physiological monitoring services are not a replacement for in-person visits. Instead, RPM is an approach that enhances patient care by addressing potential issues between visits. These services utilize FDA-cleared medical devices to monitor a patient’s health for at least 16 days per month.
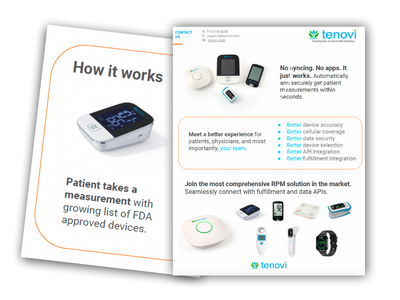
These FDA-cleared medical RPM devices include pulse oximeters, blood glucose meters, blood pressure monitors, thermometers, peak flow meters, weighing scales, and additional devices. Some devices may be familiar to patients, while others may require training and support. Providers should walk their patients through operating the device in a telehealth appointment. In addition, they may provide them with written instructions or videos.
Patient vital sign data is collected and transmitted directly to the patient’s physician. Then, the data is analyzed, and the physician is promptly notified if any readings fall outside the predetermined parameters. Medicare updated CPT 99457 to allow services that don’t require physician knowledge to be outsourced to third-party vendors. With outsourcing physicians, there’s no need to increase clinic workload or hire more staff. Instead, qualified staff can perform some RPM services such as technical support or fulfillment of devices.
Key Points
The benefits of remote patient monitoring extend to both patients and providers by reducing healthcare costs, increasing access to care, enhancing patient engagement, and improving the quality of care. Providers who want to implement RPM in their practice should be aware of the CMS policies and reimbursement CPT codes for RPM services, as well as the best practices and tips for leveraging RPM technology. By incorporating remote patient monitoring, healthcare teams can focus on improved care between in-person visits while extending quality care to more patients.
Implementing RPM provides patients with increased communication channels, fostering adherence to treatment plans and chronic condition management. This enhanced connectivity enhances patient engagement and promotes better health outcomes. Chronic care, telehealth, and RPM software and services companies can discover how Tenovi can help improve your efficiency, outcomes, and revenue by scheduling a demo today. You can see how Tenovi can transform your partner’s healthcare delivery.