A few major differences exist between remote patient monitoring and telehealth. This article outlines key differences in Medicare reimbursement protocols between telehealth and RPM services. It also identifies the 3 major differences between Medicare billing for remote patient monitoring services vs. telehealth services.
The differences between remote patient monitoring and telehealth vary depending on who defines the terms. Many people consider remote patient monitoring a type of telehealth service. However, the Centers for Medicare and Medicaid Services (CMS) does not.
What’s the Difference Between Remote Patient Monitoring and Telehealth?
Both remote patient monitoring and telehealth services involve using technology to provide healthcare services at a distance. Specifically, Telehealth, also called telemedicine, allows healthcare providers to offer virtual care for patients without an in-person office visit. Telehealth visits primarily occur online with a digital device like a computer, tablet, or smartphone.
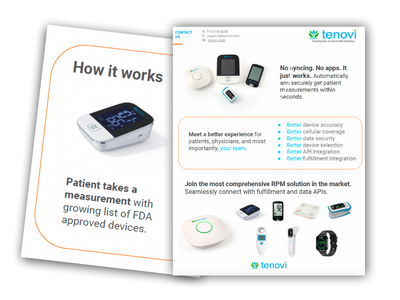
By comparison, remote patient monitoring, sometimes called remote physiological or remote monitoring, also allows healthcare providers to monitor certain aspects of a patient’s health outside the doctor’s office. RPM lets providers remotely manage acute and chronic conditions, receiving and reviewing patient vital signs in a digital RPM platform. Patients take their measurements from home with an FDA-cleared wireless medical device, such as a blood pressure monitor, scale, blood glucose monitor, and pulse oximeter. The measurement is then automatically digitally transferred to the physician.
CMS sets very strict reimbursement guidelines for telehealth services. Since CMS does not consider remote patient monitoring a telehealth service, it allows for a more flexible reimbursement protocol for RPM services. Remote patient monitoring pairs well with telehealth when a patient requires regular vital sign monitoring for certain health conditions. Additionally, clinicians can set measurement thresholds. The platform automatically alerts the physician if a patient’s reading exceeds the set limits.
The following sections highlight the 3 major differences between Medicare reimbursement for remote patient monitoring services vs. telehealth services.
1. Type of Service
Remote health encompasses remote patient monitoring and telehealth services. These are similar in that they both require interactive communication with the patient. However, the time spent interacting with a patient for an RPM service is not explicitly stated.
This means that the physician, qualified healthcare professional, or clinical staff member can divide the time spent on the type of remote monitoring service between data review and interaction with the patient. For example, below you will find more specifics on the time increments for RPM billing.
CPT code 99457 and is used for additional increments of 20 minutes after the initial 20-minute minimum has been met. Every 20 minutes of remote treatment services by clinical staff/physician/other qualified health care professional time. It requires interactive communication with the patient or caregiver during the month. The first 20 minutes one billable unit of time each 30 days.
CPT code 99458 is an add on code to CPT 99457. It is used for additional increments of 20 minutes after the initial 20-minute minimum has been met, and is billed in 20-minute increments each month.
CPT Code 99091 is used for collection and interpretation of physiologic data transmitted to the physician or other qualified health care professional, requiring a minimum of 30 minutes of time, each 30 days. Healthcare organizations cannot bill CPT codes 99091 and 99457 together for the same billing period.
Remote physiological monitoring services are not a substitute for in-person visits. Rather, they focus on providing better care between visits to catch complications early and prevent them from worsening. Remote patient monitoring requires using FDA-cleared medical devices to monitor a patient’s health for at least 16 days per month. The RPM device analyzes information after gathering it and immediately alerts the physician when a reading is outside the set parameters.
In contrast, telehealth services are generally meant to substitute for an in-person visit and require live, virtual, interactive communication via video or audio call. The reimbursement amount for telehealth services is the same as face-to-face in-person services. Every 20 minutes of data review for RPM services comprises 1 billable unit.
2. Location
Telehealth services have originating site requirements. An originating site is where the patient is at the time of service. The patient must go to the designated originating site to receive telehealth services in a county outside a Metropolitan Statistical Area (MSA) or a rural Health Professional Shortage Area (HPSA).
Authorized originating sites include:
- Physicians or practitioner offices
- Hospitals
- Critical access hospitals
- Rural health clinics
- Federally qualified health centers
- Hospital-based or CAH-based Renal Dialysis Centers
- Skilled nursing facilities
- Community mental health centers
In contrast, remote patient monitoring services do not have originating site requirements. Instead, patients can take their vital sign measurements from the comfort of their own homes or locations of choice.
3. Service Provider
Another crucial distinction between remote patient monitoring and telehealth is who can provide the services. Eligible telehealth service providers include:
- Physicians
- Nurse practitioners
- Physician assistants
- Clinical nurse specialists
- Nurse midwives
- Clinical psychologists
- Clinical social workers
- Registered dietitians or nutrition professionals
In contrast, RPM services can be performed by a physician, qualified healthcare professional, or clinical staff. RPM services can be billed ‘incident-to’ and performed under the ‘general supervision’ of the billing physician. This enables clinicians to hire third-party remote patient monitoring companies for general data review services.
Subsequently, RPM is accessible to more people. This enables clinics to manage more patients and generate increased revenue without significantly impacting workflows. In fact, one large Federally Qualified Health Center’s reduction in missed appointments has translated into cost savings. The revenue from averted no-show appointments totaled $45,578 per month.
Remote Patient Monitoring and Telehealth: Benefits and Summary
Many people still consider remote patient monitoring a type of telehealth service. However, Medicare does not include remote patient monitoring in its list of telehealth services. This allows clinicians to utilize more flexible reimbursement terms to improve patient outcomes.
Telehealth services increased dramatically during the COVID-19 pandemic. In the following states alone: Arizona, California, Maine, Mississippi, and Missouri, telehealth services grew 15x the pre-pandemic level (from 2.1 million the year before to 32.5 million in the 12 months from March 2020 to February 2021). Benefits of telehealth include:
- Increased access to care for those in remote areas or with limited mobility
- Convenience of appointments from home, reducing time off work
- Ability to follow up with brief check-ins as needed
The advancement in digital health technologies is growing awareness among providers and patients. As telemedicine becomes more widely available, remote patient monitoring also does. More healthcare providers are offering RPM because it allows monitoring for patients with chronic conditions and prevents serious complications for those in remote or rural locations.
According to the U.S. Department of Health & Human Services, the benefits of remote patient monitoring include:
- Reduced hospitalizations
- Shorter hospital stays if the patient can be discharged with a remote monitoring device to use at home
- Fewer visits to the emergency room
- Better health outcomes for patients in rural areas
- Better preventative management for chronic conditions
- Reduced risk of COVID-19 exposure, along with other illnesses, for patients and health care workers
Are you considering remote patient monitoring? Tenovi RPM devices are easy to use for patients. There is no syncing and no app required. Physicians automatically and securely get patient measurements within seconds. Schedule your free demo and consultation today.