Heart disease remains the leading cause of death in the United States, claiming nearly a million lives in 2020 alone. Beyond the emotional toll, heart disease exerts a considerable financial strain on patients and their families. From 2019 t0 2020, heart disease cost about $252.2 billion. Yet, what makes heart disease particularly dangerous is that it often progresses silently until a major cardiac event strikes. Today, healthcare providers are increasingly turning to remote patient monitoring (RPM) for heart disease as a powerful tool to manage heart conditions more proactively.
By leveraging connected devices that track vital signs like blood pressure, glucose levels, and weight, RPM allows providers to monitor patients between visits, detect early warning signs, and intervene before complications escalate. But how effective is cardiac RPM? Can it improve outcomes and reduce costs for patients living with cardiovascular disease?
In this article, we explore the latest research on remote patient monitoring for heart disease, including its role in preventing hospital readmissions, improving access to care, and supporting high-risk populations like heart failure and diabetes patients. We also break down the devices that power these programs—and what healthcare organizations should know when choosing an RPM solution.
Remote Patient Monitoring for Heart Disease Patients
Unfortunately, often with heart disease, there are no symptoms until a heart attack, heart failure, or arrhythmia strikes. This is why high blood pressure is called the “silent killer.” A healthy lifestyle includes no smoking, regular exercise, a balanced diet, and heart health. Protecting patients from these hidden dangers requires heightened awareness of risks, lifestyle changes, and frequent blood pressure monitoring.
This sobering reality propelled Ahmed Fawzi Otoom and a team of researchers to develop a continuous, real-time remote patient monitoring system designed to monitor the heart. His objective was to identify and address any cardiac issues promptly. Since 2014, remote patient monitoring technology has advanced, particularly for chronic cardiovascular conditions.
Today, researchers continue exploring new possibilities to enhance cardiac care. The use of FDA-cleared cardiac remote patient monitoring devices offer an effective means for providing comprehensive insights into patients’ cardiac health. The following section explores how remote patient monitoring is used for heart disease.
Remote Patient Monitoring and Heart Disease
Remote patient monitoring is a form of telehealth that utilizes IoT technology to transmit physiological measurements from a patient to their healthcare provider. A robust remote patient monitoring program can empower patients with heart disease to actively participate in managing their health. RPM gives physicians a full view of patient vital signs between in-office appointments and heart health over time. In addition, when used appropriately, RPM enables increased understanding of a patient’s adherence to treatment and timely intervention.
Cardiac remote patient monitoring is a valuable tool for regularly monitoring heart conditions. Monitoring blood pressure outside of a medical setting is known as remote blood pressure monitoring. A significant contributing factor to heart disease is high blood pressure, also known as hypertension. High blood pressure can damage arteries by making them less elastic, resulting in decreased blood and oxygen flow to the heart. This can lead to heart disease in addition to serious health problems such as:
- angina/chest pain
- heart attack
- heart failure
- stroke
- kidney disease
Complications From High Blood Pressure
To understand cardiac health comprehensively, it’s crucial to recognize three distinct yet interrelated conditions: angina, heart attack, and heart failure. Together, these conditions illustrate a comprehensive picture of the intricate world of cardiac health. First, angina is chest pain caused by reduced blood flow to the heart, a coronary artery disease symptom.
Second, a heart attack, a myocardial infarction, occurs when the blood supply to the heart is blocked. When this happens, the heart muscle dies due to a lack of oxygen. The longer the blood flow is blocked, the greater the damage to the heart.
Finally, heart failure is when the heart cannot pump enough blood and oxygen to the body’s other organs. 6.5 million Americans over the age of 20 have heart failure. The body depends on the heart to effectively pump nutrient-rich blood to cells because the cells need sufficient blood supply to function correctly.
RPM in Stroke Prevention
Furthermore, high blood pressure is the leading cause of stroke. High blood pressure occurs due to extra pressure on blood vessels. Over time, a blood vessel may not withstand the extra pressure. As a result, the blood vessel can rupture, causing a hemorrhagic stroke. In addition, high blood pressure may cause artery walls to thicken. This narrows the space available for blood to pass, which increases the chances of blockage that can cause ischemic stroke.
With remote patient monitoring for heart disease, a clinician can set and receive real-time alerts when a patient’s blood pressure is too high. Patients want to aim for a blood pressure reading of less than 130/80 mmHg. Anything above that is considered hypertensive and increases the risk of stroke. Clinicians can use cardiac remote patient monitoring to monitor trends in blood pressure readings and observe how patients respond to medications.
Heart Disease Prevention: Remote Blood Glucose Monitoring
Diabetes patients are twice as likely to develop heart disease or stroke than those without diabetes. In the U.S., diabetes is the seventh leading cause of death, with 65% of deaths attributable to cardiovascular disease or stroke. If not properly managed, this costly disease can lead to:
- heart attack
- kidney failure
- blindness
Diabetes can also be managed with remote blood glucose monitoring. That way, a qualified healthcare professional consistently monitors blood glucose levels. Patients should aim for a blood glucose reading between 80-130 mg/dL before a meal and below 180 mg/dL two hours after a meal. Regular blood glucose monitoring keeps patients involved in managing their health. When patients regularly take their vital signs, they see how diet, physical activity, medications, and stress affect their blood glucose levels.
Cardiac Remote Patient Monitoring Devices
Remote patient monitoring devices take vital sign measurements and transmit them to physicians in real-time. A host of FDA-cleared devices are available for remote cardiac monitoring. For example, some devices include implantable biosensors; others may consist of blood pressure monitors, blood glucose monitors, and pulse oximeters. The following section explains the differences between invasive and noninvasive cardiac remote monitoring devices.
Invasive Remote Heart Monitoring Devices
Some cardiologists may use invasive remote heart monitoring devices with biometric sensing. This requires the implantation of an internal device that continuously monitors and collects data. Two typical devices are implantable hemodynamic monitors and cardiovascular implantable electronic devices—for example, a pacemaker or defibrillator. The first implant of a cardiac pacemaker occurred in 1958. Over several decades, significant improvements have led to the creation of noninvasive remote heart monitoring devices.
Noninvasive Remote Heart Monitoring Devices
Now that we have explored active and passive remote patient monitoring in heart disease, we have turned to noninvasive cardiac devices, also known as external devices. Unlike implantable electronic monitoring devices, noninvasive remote heart monitoring devices can be active or passive. Active approaches might be stepping on a scale to obtain a weight measurement. An example would be remote hemodynamic monitoring that involves the continuous assessment of blood flow, pressure, and oxygenation within the cardiovascular system.
While passive approaches secure data without the patient taking any action. For instance, a bed sensor may measure a patient’s RR interval automatically. Next, we’ll explore noninvasive cardiac remote blood pressure monitor devices called external devices.
Wireless Blood Pressure Monitors
Depending on the patient’s heart condition, the RPM device used will vary. For example, a hypertensive patient may use a wireless blood pressure monitor, while a diabetic patient may use a wireless blood glucose meter. Patients enrolled in remote patient monitoring programs must use their device for at least 16 days out of the month.
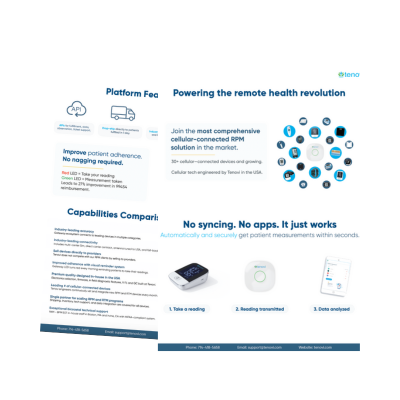
Once the reading is taken, the remote patient monitoring device sends the vital sign data in real-time to an RPM platform. The clinician then accesses the data from the RPM dashboard and acts upon the results as necessary. It is important to note that clinicians can set thresholds to receive timely alerts. The platform automatically alerts the physician if a patient’s reading exceeds the specified limits.
Wireless Blood Glucose Meters
Since cardiovascular disease is more common in patients with diabetes, wireless blood glucose meters may be prescribed to a patient. RPM devices ensure a patient’s blood glucose levels are consistently monitored. This technology helps clinicians see what may or may not be working and adjust patient treatment plans. Physicians can set thresholds and receive an alert when fluctuations in readings occur. Virtual cardiology care providers can promptly take appropriate actions to treat their patients.
Patients are responsible for taking measurements at least 16 days a month, and care providers monitor their daily readings. Therefore, patients are more likely to follow their treatment plans and adopt healthier behaviors. A Journal of Diabetes Science and Technology study found that remote patient monitoring interventions that incorporate key elements of structured self-monitoring of blood glucose (SMBG ) appear to have the most significant impact on A1C levels.
Remote Weight Monitoring in Congestive Heart Failure
Weight gain is often one of the first signs of congestive heart failure. Regular body weight readings can identify if a patient’s heart failure is worsening or if adjustments are needed to control fluid retention. This is not the only way to manage congestive heart failure. However, daily weigh-ins help provide a more accurate understanding of their patient’s health.
When a patient’s weight fluctuates by more than 3 pounds in a single day, their remote weight monitoring device can send a real-time alert to the clinician. Remote patient monitoring studies dating back to 2011 suggest that patients monitored remotely are less likely to have readings fall outside a healthy range. Daily weight monitoring allows patients with congestive heart failure to work on preventative care rather than treatment.
Remote Patient Monitoring for Heart Disease and Effectiveness
RPM allows patients to stay home and follow their daily routines. For patients with cardiovascular diseases such as congestive heart failure, remote patient monitoring strategies enable physicians to identify and preempt potentially dangerous and costly emergencies. Healthcare teams can quickly react to small and significant changes in the patient’s daily vital sign monitoring.
An RPM in cardiac care study showed a 65% reduction in hospital admissions and an 85% decrease in inpatient services for patients enrolled in a Virginia medical network’s nursing and RPM program. The decline in admissions and services resulted in $615,127 in patient claims cost savings.
Reduced Readmissions in Congestive Heart Failure Patients
If remote patient monitoring interventions are designed with patients, providers, and the implementation setting in mind, they will more likely be effective at reducing acute hospital events. Chronic and acute care patients account for the highest population experiencing readmission to hospitals in the U.S. Congestive heart failure poses the highest risk of readmission to the hospital. One in four patients with heart failure is readmitted within the first 30 days of discharge, with 50% readmitted within six months.
Remote patient monitoring reduces readmissions, adding to value-based care while increasing health outcomes in patients with heart disease. A single-center study conducted in 2017 found that a remote patient monitoring program for heart failure coupled with unstructured education, remote patient monitoring devices, and alert-specific medication reduced the likelihood of experiencing a cardiac hospitalization and cardiac-related emergency department visit.
Increased Medical Access in Rural Areas
A study published in Health & Technology states that in rural areas, people die early because of a lack of proper facilities and infrastructure for monitoring patients’ health at the right time. Therefore, developing telemedicine and remote patient monitoring technology is significant in rural areas.
Telehealth and remote patient monitoring expand access to preventive care in unassisted populations for chronic disease, such as those with heart disease. Medicare recipients are eligible for RPM services, provided the device can reasonably apply to treatment for the patient’s condition.
This means patients in rural areas can be less concerned with finding transportation from their appointments. Telehealth and remote patient monitoring together have the potential to bridge the gap of lack of access and transportation for people in rural areas to meet their timely healthcare needs.
RPM and Cost Effectiveness
High hospital readmission rates heighten the economic burden of heart failure. The readmission rate for chronic conditions was so concerning that the Hospital Readmission Reduction Program (HRRP) was introduced in 2012. HRRP penalizes hospitals for excessive rates of readmission for the following conditions: heart failure, acute myocardial infarction (AMI), pneumonia, chronic obstructive pulmonary disease (COPD), coronary artery bypass graft (CABG) surgery, and hip or knee replacement.
A 2021 study evaluated the cost-effectiveness of telehealth with remote monitoring for postpartum pregnancy monitoring for hypertensive disorders. Ultimately, the study suggested that with a cost savings of $93 per patient and an estimated 333,253 pregnant women with hypertension in the U.S. per year, telehealth could reduce healthcare costs in the U.S. by approximately $31 million a year.
Clinical efficiency
Healthcare organizations must understand how to set up an efficient remote patient monitoring workflow. In this way, healthcare providers experience minimal impact on clinical workflows. This is because remote patient monitoring allows clinicians to prioritize healthcare delivery, scrutinize each patient’s real-time status, and respond accordingly.
With healthcare staffing challenges, remote patient monitoring helps reduce increased workloads and in-person visits because medical teams can provide some virtual care services. RPM can result in increased revenue for healthcare organizations.
Outsourcing RPM Services
Healthcare organizations can bill for remote patient interactions, adding to an organization’s bottom line. RPM CPT codes 99458 and 99457 allow physicians to reimburse for time spent on RPM services like patient data collection and review. With remote patient monitoring, clinicians can care for more patients without necessarily spending more time. However, healthcare organizations can also outsource remote patient monitoring services.
Using a third-party remote patient monitoring company can minimize the time it takes for staff to adjust existing workflows. Tenovi RPM offers an accurate and easy-to-use solution to boost workflow efficiency and patient satisfaction and generate revenue. Schedule a free demo, and get ready to meet a better RPM experience with Tenovi.